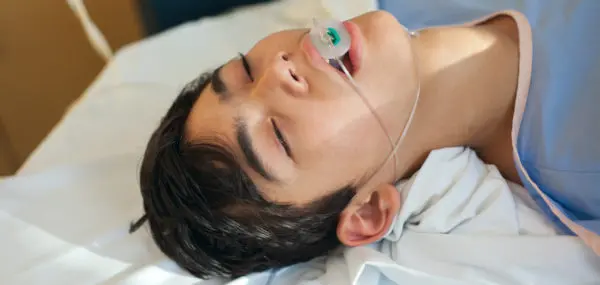
If your teenager has had wisdom teeth removed, it’s possible the dentist sent them home with a prescription for an opioid such as Percocet (oxycodone) or Vicodin (hydrocodone). While these medications do, indeed, relieve pain and discomfort, they still must be carefully considered.

Risks of Opioid Painkillers:
While opioids are effective for treating pain, they may not be necessary. A study has found that they are no more effective than non-opioids. (In this study, they were specifically tested in treating back, hip, and knee pain.)
Prescription opioids were developed to treat severe pain, but in the past two decades, they have been marketed for widespread use.
The rapid-release painkillers are chemically similar to endorphins, the body’s natural pain reliever. Opioids also release the hormone dopamine, which creates a feeling of euphoria.
Most concerning is that they pose a huge risk for kids who may start off taking them for legitimate pain relief, but get hooked. There is no getting around the fact that opioids are extremely addictive.
“Teenagers are playing Russian roulette,” says Donlon Wade, who has been a teen substance misuse counselor for over 40 years. “They take one pill and get a pretty good high, and it either scares them away because the cravings come so quickly—or, instead, they want to repeat the euphoria.”
Consequences:
When the bottle of pills is gone, the addiction continues. This can lead the teen down even more dangerous paths. Wade treated a teenage girl from an affluent community who sold everything in her home while her parents were away in order to buy opioids, which cost at least $1 per milligram on the street. In extreme cases, this can translate into an $80-per-day (or more) habit.
“We often see patients who may have started using prescription opioids and then start using heroin or fentanyl because it’s less expensive and gets to a more potent high,” says Sarah Bagley, a pediatrician and specialist in adolescent addiction at the Grayken Center for Addiction at Boston Medical Center.
Opioid Addiction Prevention:
1. Consult with the doctor.
If your child is having surgery, talk to the doctor about whether they actually need a narcotic. Dr. Bagley says it’s perfectly reasonable to have that conversation with your provider and share in the decision.
“There are still going to be times when opioids are indicated,” says Dr. Bagley. “We don’t want teens or other people to be in pain, but there are times when we can treat with non-opioid medication.”
2. Keep track of the medication.
If the doctor does prescribe an opioid, keep careful track of the pills.
“Parents can play a really important role by being aware of how many pills are prescribed, keeping them in a secure location, and monitoring what their child is taking,” says Dr. Bagley. “Once the pain is resolved, you really want to take those extra pills and dispose of them.”
Police departments, pharmacies, or city offices often have safe depositories to dispose of leftover or excess prescription medications.
3. Be aware of warning signs of opioid use.
Wade says the signs that indicate opioid abuse are the same as for other types of drugs or alcohol.
“If grades start going, if money starts disappearing, if their attitude changes, if secrets start flying, you’ve got some issues,” says Wade.
Dr. Bagley says that if you notice changes in behavior, then you should work with a healthcare professional to figure out what’s going on. Your child may have become more withdrawn and moody for other reasons—depression or anxiety, for instance—but you won’t know until you investigate.
“It can be hard; you need to trust your parental gut,” says Dr. Bagley.
4. Communicate with your child.
An open, honest relationship with your child is the best preventative measure you can take, both experts say.
“They need to be able to talk to you in a way that’s safe, so they are not going to be punished about what they share,” says Dr. Bagley.
It’s also important to continue providing structure. Be aware of where your child is after school and on the weekends. Set rules and stick to them.
“Something that will really help is the quality of the relationship you have with your child,” says Wade. “If you’re not in communication, and not doing things with them, you have a good chance of never knowing all this stuff is happening.”
Opioid Addiction Treatment:
Dr. Bagley stresses that it’s important for parents to understand that addiction is a disease, not a moral failing, and that treatment works.
“When families are in the throes of this, they forget that teens can get better—do get better,” she says. “But it’s a condition that’s going to require continuing care over time.”
If you suspect your teen is using opioids, reach out to your family medical provider, who may refer you to a substance misuse counselor, or an organization that offers support to addicted people and their families.
Above all, do something. Ignoring the problem will not make it go away.
Opioid Addiction Resources:
Substance Abuse and Mental Health Services Administration (SAMHSA) has a Behavioral Health Treatment Services Locator on their website at findtreatment.samhsa.gov. Their hotline, 1-800-662-HELP (4357) offers free, confidential information in English and Spanish for individuals and family members facing substance abuse and mental health issues 24 hours a day, 7 days a week.

For more information, also see National Institute on Drug Abuse (nida.nih.gov) and Partnership for Drug Free Kids (drugfree.org).